Announcements
Relationship between microbiota and mental health
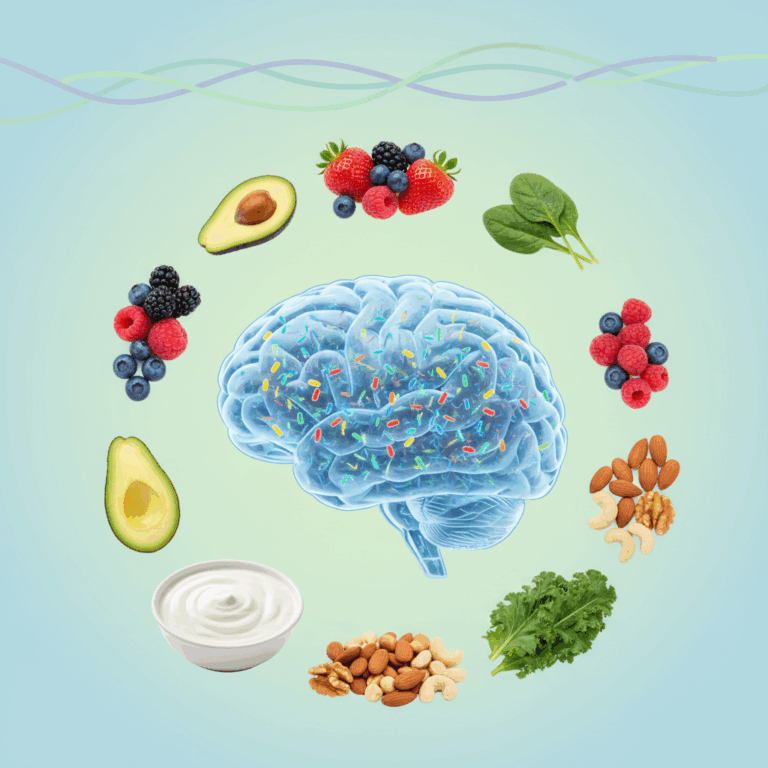
The intestinal microbiota it plays a fundamental role in mental health through the microbiota-gut-brain axis, a two-way communication network that connects the gut to the brain. This axis directly influences emotions and mood through multiple pathways.
Transmitted signals include the vagus nerve, the immune system, and the production of key neurotransmitters. Thus, the microbiota can affect brain function and emotional regulation, evidencing its importance in mental health.
Microbiota-gut-brain axis and its communication pathways
Announcements
The microbiota-gut-brain axis is a complex network where the intestinal microbiota interacts with the central nervous system. Communication occurs through nervous, immunological and metabolic pathways, integrating signals that modulate the brain.
The vagus nerve acts as the main channel, transmitting information from the intestine to the brain and vice versa. In addition, the immune system regulates the inflammatory response, key to mental and emotional health.
Announcements
This axis allows changes in the microbiota, such as dysbiosis, to alter cognitive function and mood, demonstrating a close connection between the body and psychological well-being.
Neurotransmitters involved and emotional regulation
The microbiota influences the production of neurotransmitters essentials such as serotonin, dopamine and GABA, which regulate mood, anxiety and emotional behavior. These chemicals are key to maintaining emotional stability.
For example, mood-modulating serotonin is largely generated in the gut, relying on a healthy microbiota for its proper synthesis. This demonstrates the importance of microbial balance for mental health.
Alterations in the microbiota can reduce neurochemical production, favoring disorders such as anxiety and depression. Thus, emotional regulation is directly influenced by the quality and diversity of the intestinal microbiota.
Impact of dysbiosis on mental disorders
The intestinal dysbiosis, an imbalance in the microbiota is associated with alterations in mental health. This phenomenon can trigger or aggravate disorders such as anxiety and depression.
Changes in microbial composition affect neurotransmitter production and inflammation, directly influencing mood and brain function, showing the importance of maintaining a balanced microbiota.
Microbial imbalance and its association with anxiety and depression
The reduction of beneficial bacteria and the increase in pathogenic microorganisms cause a microbial imbalance which is linked to symptoms of anxiety and depression. This imbalance modifies communication in the intestinal-brain axis.
Studies indicate that dysbiosis can alter the production of serotonin and other fundamental neurotransmitters, negatively influencing emotional regulation and promoting the appearance of mental disorders.
Chronic inflammation and intestinal permeability induced by stress
Prolonged stress can increase the intestinal permeability, allowing toxins and bacteria to enter the circulation. This generates chronic inflammation, affecting both the central nervous system and emotional well-being.
The inflammation caused by this permeability can deregulate brain function and increase vulnerability to conditions such as depression, showing a clear relationship between intestinal and mental health.
Effects on the central nervous system and mood
Dysbiosis and intestinal inflammation impact the central nervous system by modifying the production of neurotransmitters and activating immune responses that influence mood.
These effects can manifest as alterations in emotional behavior, reducing the ability to manage stress and increasing susceptibility to mental disorders.
Research and evidence on emotional microbiota
Numerous scientific studies they have explored the relationship between gut microbiota and emotional modulation, using both animal and human models to understand these mechanisms.
This research has shown that microbial composition can significantly influence emotional behavior, opening avenues for novel treatments based on intestinal health.
Studies in humans and animal models on emotional modulation
Research in animal models has shown that altering the microbiota modifies behavior, reducing anxiety or improving the stress response. This reflects a causal connection.
In humans, emotional changes associated with microbial composition have been observed, where a balanced microbiota is related to more stable moods and a lower incidence of disorders.
The mechanisms involve the production of neurotransmitters by the microbiota, as well as modulations in the immune system, which directly affect brain and emotional function.
Specific probiotics and their influence on depressive symptoms
Some strains of probiotics, such as Bifidobacterium and Lactobacillus, have been shown to reduce depressive symptoms by improving intestinal barrier function and decreasing systemic inflammation.
These probiotics act by promoting the production of neurotransmitters related to emotional well-being, such as serotonin and GABA, helping to improve mood.
Clinical studies have reported improvements in quality of life and reduction of anxiety and depression in patients who consume these supplements, evidencing their therapeutic potential.
External factors that affect the microbiota and mental health
The intestinal microbiota can be altered by various external factors that directly impact mental health. Among the most relevant are diet, the use of antimicrobials and sleep quality.
These elements influence the composition and functionality of the microbiota, affecting its ability to regulate the microbiota-gut-brain axis and, therefore, emotional and cognitive well-being.
Diet, antimicrobials and sleep quality
An unbalanced diet, low in fiber and rich in processed foods, can harm microbial diversity, damaging the production of neurotransmitters essential for mental health.
On the other hand, frequent and unnecessary use of antimicrobials can cause severe dysbiosis, eliminating beneficial bacteria and promoting intestinal inflammation that affects mood.
Sleep quality is also key to maintaining a balanced microbiota. Lack of rest alters the circadian rhythm, altering intestinal function and promoting states of anxiety and stress.
Promotion of a healthy microbiota for emotional well-being
To promote a healthy microbiota, it is essential to adopt eating habits rich in fiber, vegetables, probiotics and prebiotics. These foods promote the growth of beneficial bacteria.
In addition, reducing unnecessary use of antibiotics, controlling stress and maintaining restful sleep contribute to preserving bacterial diversity, which is reflected in a better emotional state.
Key facts about the microbiota and emotional well-being
Recent studies show that implementing changes in diet and lifestyle can improve depressive symptoms by up to 30%, underlining the importance of taking care of the microbiota.
Therefore, taking measures to maintain intestinal health is a promising strategy to improve emotional quality of life and prevent mental disorders.